Headless Compression Screw 4.5 mm and 6.5 mm
Fixation of small and large bone fragments require meticulous reconstruction of the articular surface while preserving the surrounding cartilage and soft tissues. In order to achieve stable fixation with primary bone healing, the application of suitable controlled compression is preferred to support a high clinical success rate. Standard screws are problematic in intraarticular applications and in areas with little soft tissue coverage. Protruding heads may damage the joint surface or irritate soft tissue. Therefore, an adequately sized lag screw would be beneficial, one that could be buried below bone surface, for example, in the knee, ankle and foot.
The headless compression screw (HCS) 4.5 and 6.5 function the same way as the existing HCS 2.4 and 3.0. The design of the HCS 4.5 and 6.5 is specifically adapted to treat fractures, osteoarthritis or deformities of small to large bones. The HCS 4.5 is primarily intended for the calcaneus, talus, metatarsus, distal and proximal tibia, distal femur, as well as proximal humerus. The HCS 6.5 may be used for all the above except the proximal humerus.
The headless compression screw 4.5 comes in lengths of 20110 mm with short thread (shaft thread lengths 722 mm) and 30110 mm with long thread (shaft thread lengths 1244 mm).
The headless compression screw 6.5 comes in lengths of 30150 mm with short thread (shaft thread lengths 16 mm), and 45150 mm with long thread (shaft thread length 32 mm).
For the large size HCS the same instrumentation as for the existing HCS can be used. The only additional ones are the attachment for compression sleeve for powered screw insertion, drill bit for predrilling the near cortex, and sleeve for compression sleeve.
Case 1: 62-year-old white female with right stage II posterior tibial tendon insufficiency and II and III overload due to medial cuneiform first metatarsal joint instability treated with UCBL for 6 months after she complained of severe pain and increasing swelling
Case provided by Juan Bernardo Gerstner Garcs, Cali, Colombia
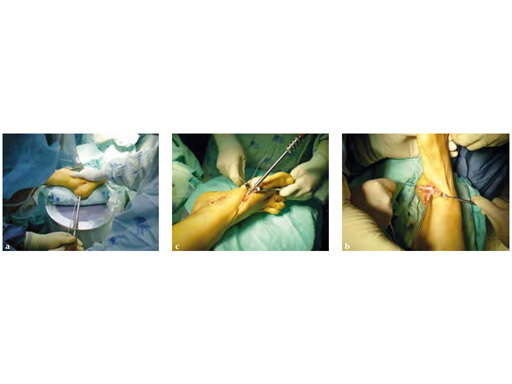
A medial displacement osteotomy of the calcaneus and transfer of the tendon of the flexor digitorum longus to the navicular fixed with an interference screw were performed (see Fig 2a-c). A fusion of the first medial cuneiformmetatarsal I, II, and III modified. Weil osteotomy was performed as well.
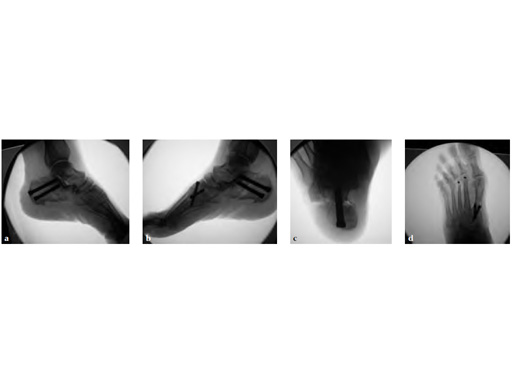
The talar axis is aligned to the midshaft of the first metatarsal (see Fig 3a-d).
Case 2: 67-year-old white female
Case provided by Juan Bernardo Gerstner Garcs, Cali, Colombia
Stage II of her left posterior tendon dysfunction and tarso/metatarsal, instability visible on x-ray (see Fig 1a-c).
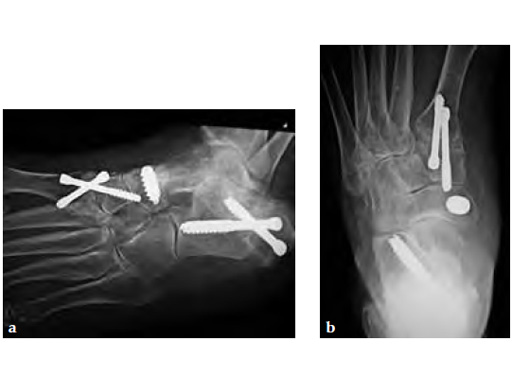
A medializing calcaneal osteotomy was performed and fixed with two 6.5 mm HCS, a flexor hallucis longus transfer to her navicular is secured with an interference 7 mm screw and a lapidus procedure fixed with two crossing 4.5 HCS (see Fig 2a-b).
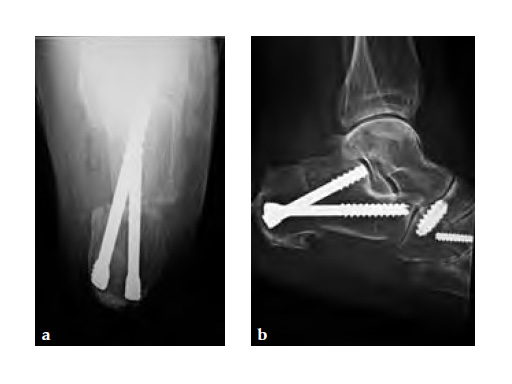
Progressive weight bearing was permitted at 8 weeks and UCBL was advised until the fourth postoperative month (see Fig 3a-b).
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO Foundation”
The brands and labels “approved by AO Technical Commission” and “approved by AO Foundation”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.