Outcomes of revision total knee arthroplasty using metaphyseal sleeves and cones
Preview
Severe bone loss is not uncommon during revision total knee arthroplasty (TKA), and often, metaphyseal fixation is critical for longer term implant survivorship. This can be achieved with implants designed for this purpose, cones, and sleeves.
Achieving stable implant fixation when the surrounding bone is compromised
According to Omar Behery, an adult hip and knee reconstructive surgeon from Charlotte, US, in a revision TKA setting, it is often difficult to rely on implant fixation at the joint surface of the femur or tibia as the host bone is often compromised.

Omar Behery
Atrium Health Musculoskeletal Institute
Charlotte, United States
The limited surface area, as well as the often sclerotic nature of the bone, are suboptimal for cemented fixation of the tibial or femoral components. In those scenarios, it is crucial to achieve fixation in the metaphysis using a cone or sleeve, together with diaphyseal fixation using a stem. Current evidence demonstrates that this improves construct survivorship compared with stemmed components alone, ie, without metaphyseal fixation. Additionally, in revision scenarios where there is significant metaphyseal bone loss, the use of cones or sleeves allows for adequate rotational control and fixation in the metaphysis, which is otherwise suboptimal. Furthermore, cones and uncemented sleeves contain porous metal surfaces which rely on biologically active osseous integration, capable of remodeling over time, which is an inherent advantage over the use of cemented components only that are prone to long-term fatigue failure. This is particularly important in younger, more active patients, who are at higher risk of aseptic failure in the long term.
Survivorship of TKA revision arthroplasty using cones or sleeves
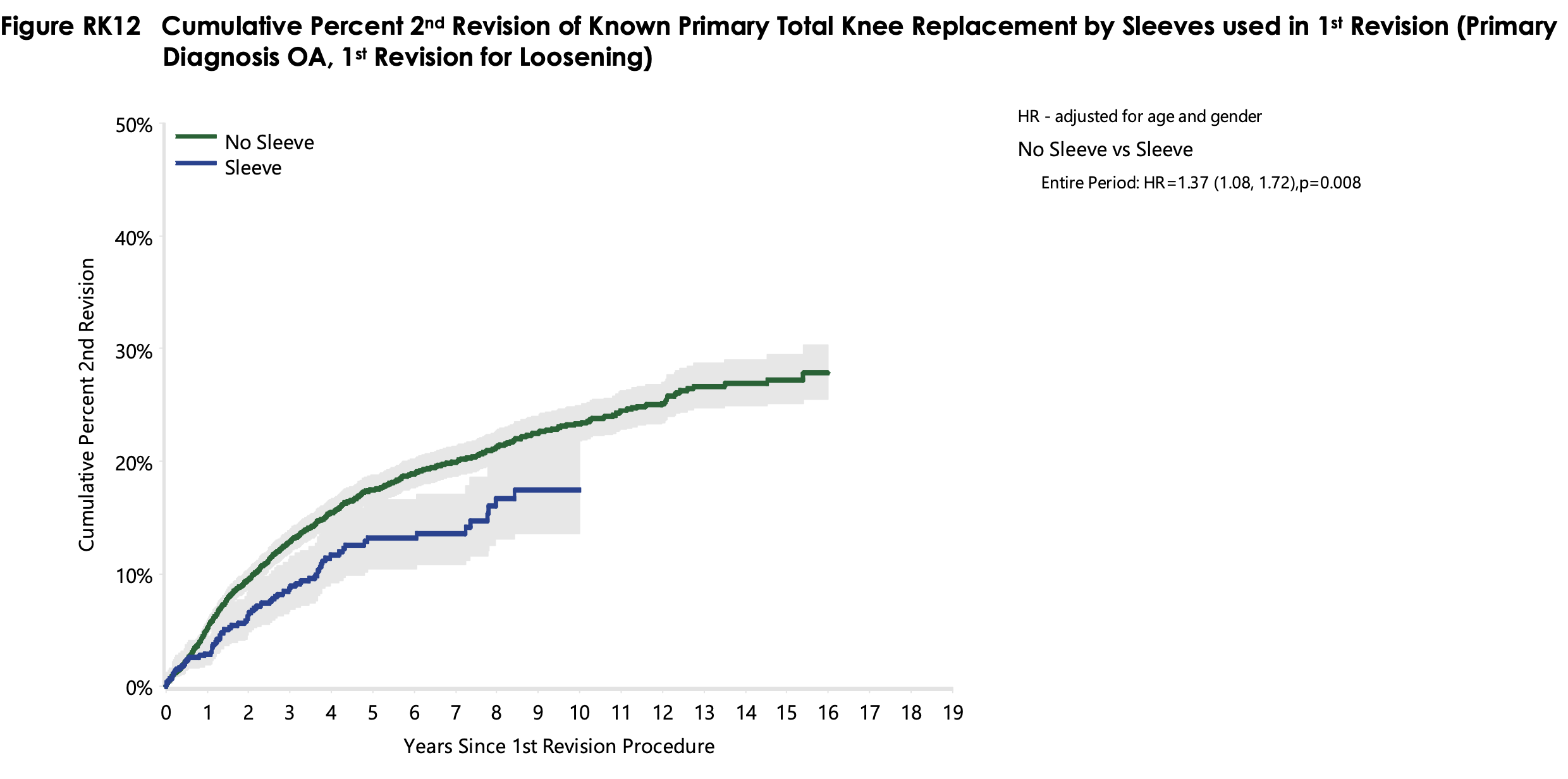
Large national joint arthroplasty registries in the UK and Australia report that the 10-year prosthetic survival rates of TKA revision surgery are around 20% [1, 2]. Nevertheless, the detailed analysis of survival rates is complex because the risk factors are manifold, and the use of sleeves and cones is just one of many variables. The National Joint Registry (NJR) of England, Wales, Northern Ireland, the Isle of Man, and the States of Guernsey [1] identified the time after primary knee replacement, type of primary fixation, type of revision prosthesis, as well as the indication for revision, as risk factors for re-revision. The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) [2] identified diagnosis, components revised, gender, age, ASA score, as well as severe obesity, as risk factors. Additionally, they analyzed the effect on re-revision rates when supplementary implants, such as stem extensions, sleeves, or cones were used. Using stem extensions or sleeves (Figure 1) resulted in improved survival rates. No such difference was observed with cones (Figure 2). However, the low number of cones in the analysis is a major limitation to this data analysis: only 79 cones were included in the beginning, and this number dropped to 23 after 3 years, and 11 cones after 5 years. Note that these analyses did not factor in the type of bone defect present at the time of surgery, as this data was not available.
Using a cone for metaphyseal anchorage of a TKA revision construct appears to affect radiographic appearance. According to Omar Behery: “Over mid-term follow-up, revision TKA constructs (femoral and tibial) with cones and short cemented stems demonstrate minimal radiolucent lines, stable radiographic appearance, and a rare incidence of aseptic loosening of a cone/short cemented construct, when compared with historic cohorts of revision TKAs using cemented or cementless stems only and no metaphyseal fixation.”
Several recent systematic literature reviews have analyzed survival rates of sleeves and cones published in various case series. The most comprehensive review was published in 2020 by Zanarito et al [3], who analyzed the results of 1,801 sleeves from 16 studies with a mean follow-up time of 4.5 years [4–19], and 927 cones from 21 studies with a mean follow-up time of 3.6 years [20–40].
They found an overall aseptic implant loosening rate of 2.2% [95% CI, 0.9–3.5] for sleeves and 2.7% [95% CI, 1.2–4.2] for cones. The overall reoperation rate was 14.4% [95% CI, 9.6–19.1] for sleeves and 17.0% [95% CI, 9.4–24.5] for cones. The revision rates, with “revision” defined as an exchange of any component (femoral, tibial, or patellar, but not polyethylene liner), were 7.5% [95% CI, 4.0–11.0] when sleeves had been used and 7.7% [95% CI, 5.0–10.4] when cones had been used. A newly diagnosed postoperative prosthetic joint infection occurred in 4.7% [95% CI, 2.5–7.0] of patients with sleeves and in 8.5% [95% CI, 5.8–11.2] of patients with cones.
Roach et al [41] published a systematic review on 1,617 sleeves from 12 studies with a mean follow-up time of 3.8 years [4–13, 16, 19], and on 701 cones from 15 studies with a mean follow-up time of 4.0 years [20, 23, 25, 26, 28, 29, 31, 32, 34–39, 42]. They reported an aseptic loosening rate of 0.8% for sleeves and 1.7% for cones along with a total all-cause reoperation rate of 9.7% for sleeves and 18.7% for cones. Additionally, they summarized information about the severity of the initial bone defects by categorizing them in either Anderson Orthopaedic Research Institute (AORI) 1/2a or 2b/3. This may be related to the severity of bone loss encountered as this analysis demonstrated that 61.7% of sleeves and 82.5% of cones were used in class 2b/3 defects. The authors caution: “It is difficult to correlate rates of aseptic loosening with degree of bone loss because not all studies specify the AORI classifications of failed implants. However, given the overall low rate of aseptic loosening in the included studies, of which included large number of defects are graded AORI 2b/3 (61.7% of sleeves and 82.5% of cones), it can be ascertained that a durable result should be expected despite degree of bone loss as measured by AORI.”
Read the full article with your AO login
- Knee function
- Pain
- Quality of life outcomes
- Intraoperative fracture
- Infection
Additional AO resources
Access videos, tools, and other assets to learn more about this topic.
- Video: Metaphyseal Fixation in Revision Total Knee Arthroplasty
- Video: Tips and Tricks to Improve Total Knee Arthroplasty Outcomes
- Video: The Difficult Primary Total Knee Arthroplasty
- AO Surgery Reference
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Omar Behery
Atrium Health Musculoskeletal Institute
Charlotte, United States

David F Dalury
University of Maryland St Joseph Hospital
Towson, United States

Glen Purnomo
St. Vincentius a Paulo Catholic Hospital
Surabaya, Indonesia

Bryan D Springer
Atrium Health Musculoskeletal Institute
Charlotte, United States

Seng-Jin Yeo
Singapore General Hospital
Singapore
This article was compiled by Elke Rometsch, Project Manager Medical Writing, AO Foundation, Switzerland.
References
- Ben-Shlomo Y, Blom A, Boulton C, et al. National Joint Registry Annual Reports. The National Joint Registry 17th Annual Report 2020. London: National Joint Registry, © National Joint Registry 2020; 2020.
- Association AO. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2020 Annual Report, Adelaide; AOA, 2020: 1–474. 2020. https://aoanjrr.sahmri.com/annual-reports-2020.
- Zanirato A, Formica M, Cavagnaro L, et al. Metaphyseal cones and sleeves in revision total knee arthroplasty: Two sides of the same coin? Complications, clinical and radiological results-a systematic review of the literature. Musculoskelet Surg. 2020 Apr;104(1):25–35.
- Agarwal S, Azam A, Morgan-Jones R. Metal metaphyseal sleeves in revision total knee replacement. Bone Joint J. 2013 Dec;95-b(12):1640–1644.
- Alexander GE, Bernasek TL, Crank RL, et al. Cementless metaphyseal sleeves used for large tibial defects in revision total knee arthroplasty. J Arthroplasty. 2013 Apr;28(4):604–607.
- Barnett SL, Mayer RR, Gondusky JS, et al. Use of stepped porous titanium metaphyseal sleeves for tibial defects in revision total knee arthroplasty: short term results. J Arthroplasty. 2014 Jun;29(6):1219–1224.
- Bugler KE, Maheshwari R, Ahmed I, et al. Metaphyseal Sleeves for Revision Total Knee Arthroplasty: Good Short-Term Outcomes. J Arthroplasty. 2015 Nov;30(11):1990–1994.
- Chalmers BP, Desy NM, Pagnano MW, et al. Survivorship of Metaphyseal Sleeves in Revision Total Knee Arthroplasty. J Arthroplasty. 2017 May;32(5):1565–1570.
- Dalury DF, Barrett WP. The use of metaphyseal sleeves in revision total knee arthroplasty. Knee. 2016 Jun;23(3):545–548.
- Fedorka CJ, Chen AF, Pagnotto MR, et al. Revision total knee arthroplasty with porous-coated metaphyseal sleeves provides radiographic ingrowth and stable fixation. Knee Surg Sports Traumatol Arthrosc. 2018 May;26(5):1500–1505.
- Gøttsche D, Lind T, Christiansen T, et al. Cementless metaphyseal sleeves without stem in revision total knee arthroplasty. Arch Orthop Trauma Surg. 2016 Dec;136(12):1761–1766.
- Graichen H, Scior W, Strauch M. Direct, Cementless, Metaphyseal Fixation in Knee Revision Arthroplasty With Sleeves-Short-Term Results. J Arthroplasty. 2015 Dec;30(12):2256–2259.
- Huang R, Barrazueta G, Ong A, et al. Revision total knee arthroplasty using metaphyseal sleeves at short-term follow-up. Orthopedics. 2014 Sep;37(9):e804–809.
- Jones RE, Barrack RL, Skedros J. Modular, mobile-bearing hinge total knee arthroplasty. Clin Orthop Relat Res. 2001 Nov(392):306–314.
- Klim SM, Amerstorfer F, Bernhardt GA, et al. Septic Revision Total Knee Arthroplasty: Treatment of Metaphyseal Bone Defects Using Metaphyseal Sleeves. J Arthroplasty. 2018 Dec;33(12):3734–3738.
- Martin-Hernandez C, Floria-Arnal LJ, Muniesa-Herrero MP, et al. Mid-term results for metaphyseal sleeves in revision knee surgery. Knee Surg Sports Traumatol Arthrosc. 2017 Dec;25(12):3779–3785.
- Stefani G, Mattiuzzo V, Prestini G. Revision Total Knee Arthroplasty with Metaphyseal Sleeves without Stem: Short-Term Results. Joints. 2017 Dec;5(4):207–211.
- Thorsell M, Hedström M, Wick MC, et al. Good clinical and radiographic outcome of cementless metal metaphyseal sleeves in total knee arthroplasty. Acta Orthop. 2018 Feb;89(1):84–88.
- Watters TS, Martin JR, Levy DL, et al. Porous-Coated Metaphyseal Sleeves for Severe Femoral and Tibial Bone Loss in Revision TKA. J Arthroplasty. 2017 Nov;32(11):3468–3473.
- Lachiewicz PF, Bolognesi MP, Henderson RA, et al. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012 Jan;470(1):199–204.
- Bohl DD, Brown NM, McDowell MA, et al. Do Porous Tantalum Metaphyseal Cones Improve Outcomes in Revision Total Knee Arthroplasty? J Arthroplasty. 2018 Jan;33(1):171–177.
- Boureau F, Putman S, Arnould A, et al. Tantalum cones and bone defects in revision total knee arthroplasty. Orthop Traumatol Surg Res. 2015 Apr;101(2):251–255.
- Brown NM, Bell JA, Jung EK, et al. The Use of Trabecular Metal Cones in Complex Primary and Revision Total Knee Arthroplasty. J Arthroplasty. 2015 Sep;30(9 Suppl):90–93.
- Burastero G, Cavagnaro L, Chiarlone F, et al. The Use of Tantalum Metaphyseal Cones for the Management of Severe Bone Defects in Septic Knee Revision. J Arthroplasty. 2018 Dec;33(12):3739–3745.
- De Martino I, De Santis V, Sculco PK, et al. Tantalum Cones Provide Durable Mid-term Fixation in Revision TKA. Clin Orthop Relat Res. 2015 Oct;473(10):3176–3182.
- Derome P, Sternheim A, Backstein D, et al. Treatment of large bone defects with trabecular metal cones in revision total knee arthroplasty: short term clinical and radiographic outcomes. J Arthroplasty. 2014 Jan;29(1):122–126.
- Fosco M, Amendola L, Fantasia R, et al. Revision total knee arthroplasty: experience with tantalum cones in severe bone loss. European Orthopaedics and Traumatology. 2013;4(3):131–136.
- Girerd D, Parratte S, Lunebourg A, et al. Total knee arthroplasty revision with trabecular tantalum cones: Preliminary retrospective study of 51 patients from two centres with a minimal 2-year follow-up. Orthop Traumatol Surg Res. 2016 Jun;102(4):429–433.
- Howard JL, Kudera J, Lewallen DG, et al. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011 Mar 2;93(5):478–484.
- Sandiford NA, Misur P, Garbuz DS, et al. No Difference Between Trabecular Metal Cones and Femoral Head Allografts in Revision TKA: Minimum 5-year Followup. Clin Orthop Relat Res. 2017 Jan;475(1):118–124.
- Schmitz HC, Klauser W, Citak M, et al. Three-year follow up utilizing tantal cones in revision total knee arthroplasty. J Arthroplasty. 2013 Oct;28(9):1556–1560.
- Villanueva-Martínez M, De la Torre-Escudero B, Rojo-Manaute JM, et al. Tantalum cones in revision total knee arthroplasty. A promising short-term result with 29 cones in 21 patients. J Arthroplasty. 2013 Jun;28(6):988–993.
- Rajgopal A, Panda I, Yadav S, et al. Stacked Tantalum Cones as a Method for Treating Severe Distal Femoral Bone Deficiency in Total Knee Arthroplasty. J Knee Surg. 2019 Sep;32(9):833–840.
- Rao BM, Kamal TT, Vafaye J, et al. Tantalum cones for major osteolysis in revision knee replacement. Bone Joint J. 2013 Aug;95-b(8):1069–1074.
- Potter GD, 3rd, Abdel MP, Lewallen DG, et al. Midterm Results of Porous Tantalum Femoral Cones in Revision Total Knee Arthroplasty. J Bone Joint Surg Am. 2016 Aug 3;98(15):1286–1291.
- Jensen CL, Winther N, Schrøder HM, et al. Outcome of revision total knee arthroplasty with the use of trabecular metal cone for reconstruction of severe bone loss at the proximal tibia. Knee. 2014 Dec;21(6):1233–1237.
- Kamath AF, Lewallen DG, Hanssen AD. Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty: a five to nine-year follow-up. J Bone Joint Surg Am. 2015 Feb 4;97(3):216–223.
- Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009 Oct;24(7):1086–1092.
- Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008 Jan;90(1):78–84.
- Mozella Ade P, Olivero RR, Alexandre H, et al. Use of a trabecular metal cone made of tantalum, to treat bone defects during revision knee arthroplasty. Rev Bras Ortop. 2014 May-Jun;49(3):245–251.
- Roach RP, Clair AJ, Behery OA, et al. Aseptic Loosening of Porous Metaphyseal Sleeves and Tantalum Cones in Revision Total Knee Arthroplasty: A Systematic Review. J Knee Surg. 2020 Feb 19.
- Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006 May; 446:83–92.
- Lai MC, Chen JY, Liow MHL, et al. Is constraint implant with metaphyseal sleeve a viable option for revision TKR with preoperative coronal plane instability and bone defect? J Orthop Surg (Hong Kong). 2020 Jan-Apr;28(2):2309499020926313.
- Denehy KM, Abhari S, Krebs VE, et al. Metaphyseal Fixation Using Highly Porous Cones in Revision Total Knee Arthroplasty: Minimum Two Year Follow Up Study. J Arthroplasty. 2019 Oct;34(10):2439–2443.
- Tetreault MW, Perry KI, Pagnano MW, et al. Excellent two-year survivorship of 3D-printed metaphyseal cones in revision total knee arthroplasty. Bone Joint J. 2020 Jun;102-b(6_Supple_A):107–115.
- Larson DJ, Rosenberg JH, Lawlor MA, et al. Pain associated with cemented and uncemented long-stemmed tibial components in revision total knee arthroplasty. Bone Joint J. 2021 Jun;103-b(6 Supple A):165–170.
- Klim SM, Amerstorfer F, Bernhardt GA, et al. Excellent mid-term osseointegration and implant survival using metaphyseal sleeves in revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020 Dec;28(12):3843–3848.
- Divano S, Cavagnaro L, Zanirato A, et al. Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg. 2018 Jun;138(6):851–863.
- Bonanzinga T, Akkawi I, Zahar A, et al. Are Metaphyseal Sleeves a Viable Option to Treat Bone Defect during Revision Total Knee Arthroplasty? A Systematic Review. Joints. 2019 Mar;7(1):19–24.