Mandibular fracture case discussion
Dr. Hopper: Hello and greetings from Seattle. I'm Richard Hopper, a craniofacial surgeon, and I'd like to introduce my colleague, Dr. Srinivas Susarla, who is a plastic surgeon and oral maxillofacial surgeon also in Seattle. We're on faculty at the University of Washington, and the purpose of this webinar, first of all, is to invite you to an exciting educational event that will be taking place on September 10th to 11th at the Hyatt Regency in Bellevue in Seattle.
It's an AO CMF NA Management of Facial Trauma course, interdisciplinary, and will cover all common fracture patterns. The second purpose of this webinar is just in the spirit of this kind of an educational event, just to have a brief case discussion between myself and Dr. Susarla on a common fracture pattern so you can get an idea of the type of learning experience that you'll be able to have in Bellevue.
Srinu, thanks very much for joining me this morning. You're on trauma call and this is a fracture pattern that anyone watching this webinar could face. They're in their first year of practice or their last day of practice, so I think it's a good one to focus on. You're on trauma call and this 36-year-old, otherwise healthy male comes into the emergency room.
He's already been worked up by the emergency room, full ATLS clearance. So no other injuries, no other medical issues that you need to worry about. He's been diagnosed already with a CT scan as having a mandible fracture. The CT scan's available to you. Maybe you could start off with letting us know how you approach this patient when you walk in the emergency room.
Having already got that information that I just gave you, do you go to the CT scan or do you go to physical examination? And in what order do you look at this kind of a patient?
Dr. Susarla: Thanks, Richard. I'd like to welcome everybody else and we hope to see you in Bellevue in September.
I think perhaps the most important thing when you're evaluating a patient like this is to trust and verify what you've been told about the patient ahead of time.
You mentioned the ATLS protocol has already been done. But just a quick survey when you evaluate the patient to immediately verify that there's no other compelling medical issues or that there is no change in the situation from the time of the trauma team or ER evaluation.
If the patient is awake and able to talk to you and doesn't appear in any kind of distress, just in a 10-15 second window, you assess the ABCDEs fairly quickly. I think the key point when evaluating trauma patients is to do it the same way every time so that you don't miss any steps. So always start with a clinical history.
Obviously, in some trauma patients, they're not going to be able to provide a history to you because of altered sensorium, or maybe they're even intubated or sedated. But in an awake patient asking about the mechanism of injury, establishing past medical history, the last 10 to 8, in case you're considering an operative intervention as well as focused complaints related to the injury.
Things like, do they have any difficulty breathing or swallowing? Do their teeth fit together? Okay. Is there any facial numbness? Are they experiencing any other symptoms that might be related to the injury? And then a focused physical examination. And again, as you pointed out, often, you get the phone call with a very specific injury that's been identified.
You're still obligated to do a comprehensive craniofacial exam because you are being consulted as the expert for the injury. And there may be some subclinical findings or otherwise relevant findings that are not included or perhaps missed. I like to do sort of a top-down exam, starting from the upper face, the midface, and then the mandible.
And again, try not to bias yourself by focusing only on the injury that's been advertised. And then once you've finished the physical exam, then go to the pertinent data, which, as you pointed out, the patient already has a CT scan. But you may also want to consider looking at laboratory evaluations as pertinent to their medical history. For example, a diabetic, you probably want to know what their blood sugars are and if there are any other compelling labs.
I think doing that through a comprehensive history, physical exam, data review, putting all that together can help you formulate a reasonable plan to manage the injury.
Dr. Hopper: That's an excellent approach. I would echo your recommendation to try to do things the same way every single time, whether it's in the emergency room or the O.R., so that you don't miss any steps. At any point when we're tired or stressed, it's easy to miss something. So you follow that algorithm that you just mentioned.
And the patient's complaining of numbness, actually, on the left side of the cheek. So not where you can see that break on the on the chin. But on the other side, he does report pretty severe malocclusion. He says my teeth, don't touch on the left side at all. He's got a little tear on Intraoral examination between the canine and the lateral incisor there.
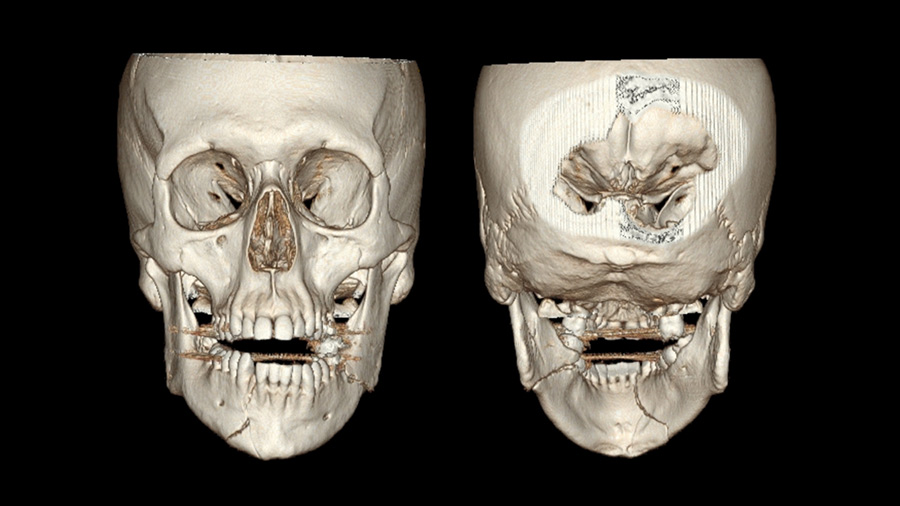
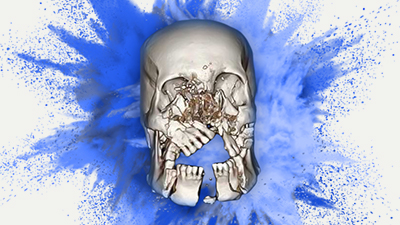
But no grossly loose teeth. Maxilla stable, the rest of the neurovascular and craniofacial examination is completely normal. What you're looking at is an mandible fracture. How did you describe this - this fracture pattern that you see in front of you?
Dr. Susarla: As you know, the first is to think is the fracture pattern concordant with the patient's clinical symptoms. The description that you provided about paresthesia and kind of the lower facial distribution that would be expected in a patient with mandibular injury because of the transit of the inferior alveolar nerve. And also coincident with the description is that gingival laceration between the right lateral incisor and the canine.
The imaging shows a right parasymphyseal fracture and a left mandibular angled fracture. And the concordance of the imaging findings with the clinical exam should be reassuring to you. Sometimes when there's a discrepancy between the two, you have to reconcile that. And one of the most important points about mandible fractures that I've learned over time and we try to stress to our own trainees is when you see a patient with what is presumed a unilateral mandible fracture, it's your job to rule out a bilateral or counter coup injury because they often occur in pairs, as you see in this case.
Dr. Hopper: Fantastic. So, you've got a pretty good appreciation of what this injury pattern is. Now, you've considered him safe from a medical and a surgical point of view for surgery. This injury just happened six hours ago. First of all: timing. Let's discuss timing. And then second: are there any options besides ORIF?
So why don't we start with timing? When do you consider treating mandible fractures?
Dr. Susarla: There's mixed data about whether waiting the usual two-week window that we might use for midface or orbital injuries impacts infection rates or outcomes in mandible fractures. My preference is to treat these injuries as soon as possible for two reasons. One, a malocclusion of this degree can be quite uncomfortable. Two, I don't worry as much about swelling in patients with mandibular fractures as I would with mid face fractures.
Generally, the mandible's easy to approach even in a swollen face. So. So I try to fix these within the first few days.
Dr. Hopper: Great, well, you're in luck. The trauma hospital's got an OR waiting for you. The patient's NPO and consent has been signed for treatment. Would you consider anything else besides open reduction, internal fixation (ORIF) or is that pretty much the one treatment that you expect to be standard in this case?
Dr. Susarla: That's a really good question. And I think for this fracture pattern in particular, I would commit fairly early to an open reduction. I don't think you could effectively treat this fracture in a closed manner. Whether that be Erich arch bars, intermaxillary fixation, or any of the hybrid systems that are now available. And the reason is with the angled fracture, you don't really have a lot of control over the proximal segment if you were to wire the patient.
Now, this fracture orientation at the angle is favorable because the angulation of the fracture runs perpendicular to the masseter muscle, so you can see on the imaging that the fracture is generally nondisplaced. A subtle finding on the imaging, which is really important, is that there is a tooth in the way of the fracture which appears to be outside of the arch alignment.
You'd have to manage that somehow as well. And I think that that would require an operative approach, it would be very hard to manage that otherwise. I would commit in this patient to an open reduction with internal fixation. And the key principle here is with these bilateral fractures, you want to have a true rigid fixation at at least one site.
The way I think about that is if you get true rigid fixation at one site, you've transitioned a bilateral fracture, to a unilateral fracture. If you do rigid fixation, say, in this case, at the parasymphysis, then maybe you can do something a little less invasive or involved for the angle.
Dr. Hopper: I think that's a great point. We were doing a few mandibles at Harborview yesterday and you're right that that intervening segment between the two mandible angles really does have also a rotational component to it. And even though you look at the CT scan and you think that that ramal side on the left side is minimally displaced, by the time you get to the operating room, that could easily be kicked laterally and not lining up.
I would agree completely with you that ORIF is really the best way to go. So, you get them into the operating room. What do you do: nasal tube, oral tube, segmental tube - what's your preference?
Dr. Susarla: My preference for isolated mandibular fracture would be a nasal tube. I think anesthesia teams at most trauma centers would be comfortable with this. But it's also an important point that craniofacial trauma management, airway management is a shared responsibility, both between the anesthetist and the facial trauma provider. So having a conversation with your anesthesia team ahead of time about the airway management as well as expectations for what should happen at the end of surgery.
For example, your anesthetist is really going to want to know, is the patient going to be wired shut at the end of the case? And if so, what are the precautions we're going to take to keep them safe during extubation as well as in the immediate recovery period? I would prefer a nasal intubation for this case. You brought up submental intubation, which is something that you can certainly consider.
I think the challenge with submental intubation in this case is with a parasymphyseal fracture like this, you might have a floor of mouth hematoma which will make navigating the tube through that submental space a little more challenging.
Dr. Hopper: I agree with that. Everybody wants to have in their little picture portfolio for presentations of submental tube and the residents love to be able to see it, but besides, that external scar and intraoral laceration can limit the movement of mobility of the mandible. I find it sometimes challenging to get the right occlusion.
You mentioned discussion with the anesthesiologist and again, that's absolutely correct. You're spinning the table patients that you intubated. Would you do arterial line for this or anything else you've talked to the anesthesiologist about steroids and then anything else that they need to know? Blood pressure?
Dr. Susarla: My preference is to use perioperative steroids. There is mixed data on that, I'll admit. But in my own practice, anecdotally, I've seen that it does make a difference, particularly in the setting of acute injuries or patients where they're not really swollen. I think once the swelling has set in, the steroids have minimal efficacy, so the usual I have them give weight-based dosing of Decadron and then perioperative antibiotics that and again remember that the perioperative antibiotics for a case like this need to cover oral flora.
So not just gram-positive coverage but also gram negative and ideally anaerobic coverage. And then I would start once the patient's intubated. I don't have specific blood pressure parameters for mandible fractures. I think you're less likely to encounter a significant hemorrhage, in contrast for some of the midface fractures, Le Fort injuries, zygoma injuries, and certainly anything inside the orbit you want to have fairly tight blood pressure control because of the risk of hematoma once the patient's asleep and you're ready to get started.
I think the first step in this case would be to apply some form of maxillomandibular fixation. My preference is to use Erich arch bars because I think they carry the advantage of being relatively inexpensive, easy to apply, and are very helpful for postoperative elastic use.
Dr. Hopper: And that's in contrast to bone anchored fixation devices, which of course tend to be quicker in less experienced hands. But do they do they come with any potential risks or complications that users need to be very aware of?
Dr. Susarla: I think in patients such as this patient where the roots of the teeth, particularly the maxilla and the anterior mandible, are in very close proximity, there is a heightened risk of the screws catching the roots of the teeth. The literature suggests that the rate of dental injury with these devices is fairly low, but I think that that's an experienced hand.
If you have any concerns about that, using Erich arch bars might be a better situation. The other thing is, with the degree of displacement in the right parasymphyseal region, you may want to consider putting on a bridle wire just to reestablish the arch integrity before trying to adapt either an Erich arch bar or a hybrid system. And then one other thing I've noticed my own practice is a lot of our patients with the hybrid systems, if they're lost to follow up or take a little longer to come back to us, sometimes there's quite a bit of mucosal overgrowth over the screw heads and it can make it a little more challenging to remove.
Dr. Hopper: When you mentioned the bridle wire to secure that dental gap. Do you prefer a bridle wire and then a single arch bar on the lower arch, or do you prefer two separate arch bars and then don't kind of join them or worry about them until the fractures are reduced?
Dr. Susarla: That's a really good question. I like to start with a bridle wire just to see if I can get the arch almost into a uniplanar occlusion and if I can and there's a fairly good adaptation of the fractured segments just with the bridle wire, then a single arch bar I think would be fine. Segmental arch bars I think are useful perhaps more so in comminuted fractures or where you have multiple segments.
But in a fracture like this where there's just a unilateral fracture within the dentate segment, I think a single arch bar would be fine. It also carries the advantage of you don't always segment the arch bar after you've exposed the fracture if you're having trouble achieving an anatomic reduction.
Dr. Hopper: This is a big topic which is teeth in the fracture line or near to the fracture line specifically the second or the third molar. So maybe we can just keep it brief, you quickly identified that there's a tooth that's an issue. Obviously, we would advise everyone not to diagnosis treatments based on purely 3D CT scans.
You're looking through your parasagittal, your coronal your axial cuts on the CT scan. What are your maybe one or two or three points where you'd say, I'm going to remove that molar before I fixate it versus I'm going to keep the tooth in there?
Dr. Susarla: I think if there's grossly visible injury to the tooth where the tooth would either be at risk of developing an infection, for example, a significant loss of coronal structure where the pulp is exposed or there's a significant aspiration risk, particularly if you're considering leaving the patient in intermaxillary fixation postoperatively. Those two situations for sure would merit removing the tooth.
And the second is if the tooth itself is interfering with your reduction and you can't find a way to reestablish the occlusion or the arch integrity based on the mouth position of the tooth, I think those scenarios would give me a sort of a very low threshold for removing that tooth. It's a little harder to see on the 3D imaging here.
But as you pointed out, the second molar on the left side appears to be significantly displaced by the fracture. And this degree of displacement of the tooth would cause me to consider removing it, which was done in this case.
Dr. Hopper: That makes a lot of sense. So just to summarize for the situation with the molar on the left: you would err towards keeping it with the exception of those issues that would either place the patient at risk or interfere with treatment and then if, as needed, deal with the molar later on.
Dr. Susarla: Right. And it is something that I think you see most frequently with angle fractures and most controversial area, and it remains controversial to this day is, what do you do with an impacted wisdom tooth that might be in the line of an angle fracture? And I don't think that there's a definitive answer one way or another. It's kind of a case-by-case basis.
You may also be interested in
AO CMF NA Computer Aided Maxillofacial Surgery (with Human Anatomical Specimens)
Dr. Hopper: So ORIF, open is the approach, R is the reduction, and then we finish off with fixation. For the open approach, would you approach these externally through the skin like a Risdon or a submental? Or would you approach them intraorally?
Dr. Susarla: I think for this specific pattern of injury, you could effectively treat it with an intraoral approach. The advantage of an intra oral approach is it spares the patient a fairly sizable submandibular incision and the associated scar as well as risk to the marginal branch of the facial nerve. The challenges with an intra oral approach in this case are navigating around the mental nerve on the right side as you're trying to get a heavy plate on the inferior border.
As well as, when you're doing angle fractures, it can be very difficult to fully see the reduction at the inferior border from an intraoral approach. And sometimes there's some splaying there. There's no ideal approach for this, but I think an intraoral approach would be my preference.
Dr. Hopper: I would agree with you, and I know what you mean about that parasymphyseal fracture, the ones that sort of arc backwards at the inferior border right underneath the mental nerve, can be challenging to get two or three good screws behind that fracture line. And like you said, you cannot always see where the plate is and you can get some palpability on the inferior border because the plate's kind of hanging low if you're not careful to make sure that's curved up correctly.
When would you use a Risdon? Obviously things like edentulous patients, things that we'll discuss at the Bellevue course, gunshots, things like that, panfaces, we often do do Risdons, but would a different kind of ramal fracture, angle fracture, push you towards the Risdon approach?
Dr. Susarla: I think in a patient where there was significant displacement or as you mentioned, some degree of comminution of the angle or the ramus where I really needed to make sure that the inferior border alignment was ideal - that would push me towards utilizing an external approach. Another situation is a third molar, where you're removing the third molar and there's a bony defect where your most reliable fixation is going to be at the inferior border.
That would be another situation where I would err towards an external approach. And you're right, I think my threshold for doing external approach to an angle fracture is actually quite low. I think if you're thinking about it, it's probably worth doing because usually your intuition is right.
Dr. Hopper: I would agree with that. You've exposed the fractures nicely through intraoral approaches and now you're trying to get your occlusion with your arch bars. You have your bridle wire in there, you're working on all the different three axes of alignment. What's the tendency for this malocclusion that you're trying to fight against?
What is it specifically that you will always keep on your radar to make sure that you're correcting as you're placing the patient into maxillomandibular fixation?
Dr. Susarla: You want to base the occlusion on wear facets. And a lot of our trauma patients, they're not like orthognathic patients. They haven't gone through presurgical orthodontic coordination, so you can't expect that the occlusion is going to be perfect.
So really relying on the wear facets, I think we'll get most of the way there and then trying to assess the concordance between the ideal fit of the teeth into their interdigitation as well as the boney anatomic alignment. The sequence is: put the arch bars on, reestablish the arch form, put the patient into maxillomandibular fixation, then expose their fractures and see how much of a discrepancy there is
between what you see at the level of the teeth and what you see at the level of the bone. Because sometimes just a minor shift at the level of the teeth can cause a major shift at the level of the bone because of the sort of lever arm and axis of rotation distance between the two.
Dr. Hopper: That sounds good. You've got the patient into a good occlusion and, and like you said, you then go back to your fractures and things like you can see that ramal segment can sometimes be kicked out and unable to be reduced. If you start to focus on your parasymphyseal fracture and you don't realize that your ramal fracture has not been reduced, then all of a sudden you have to take them out of MMF and get it reduced before you can start to work on the ramal fracture.
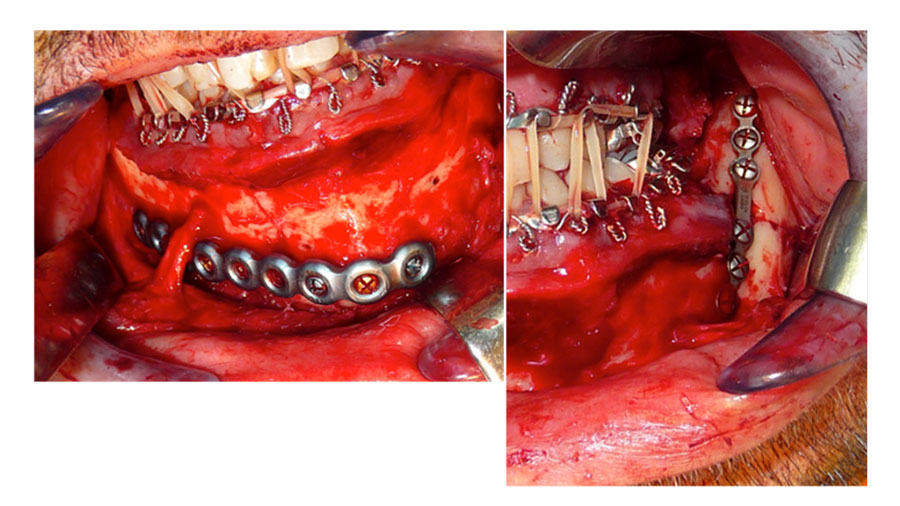
I agree, you have to have that constant back and forth between occlusion and seeing what the fractures are doing. And it's really that the big picture view that you have to keep in mind. So, you've got them into a good occlusion and these are the plates that you chose to use.
Maybe you can just briefly explain why you decided on this inferior border plate for the parasymphyseal fracture and the Champy plate for the angle fracture.
Dr. Susarla: It kind of goes back to what we were talking about earlier, is that when you have bilateral fractures at the mandible, one approach that I think works really well is to simplify the injury by putting true rigid fixation on one site so that you have a little more flexibility with the other site. In this case, we used an intraoral approach as you can see, you can see the mental nerve dissected completely free.
And then we used a heavy locking reconstruction plate for the parasymphyseal fracture with three bicortical screws on either side. The key advantage of this is this is true rigid fixation for this region of the mandible. You can essentially have the patient without an arch bar at the end of the case. If you were to use a lighter plate that didn't meet the requirements for true rigid fixation and isolation, then you might have to consider leaving a tension band on
Which would be hard in this case to put a mini plate above this because of the location of the mental nerve. And then you might be obligated to leave the arch bar on, which presents its own challenges with hygiene and using or having true rigid fixation in a parasymphyseal fracture then gives you a little more flexibility with the angle.
So as you mentioned, when we expose the angle, if you're able to get it into a good anatomic alignment with visual inspection at the superior border and either a direct inspection from an intraoral approach for the inferior border or just by palpation, you might be able to use something that would be functionally stable fixation or semi-rigid fixation, which in this case is this Champy miniplate.
Dr. Hopper: In September we'll be talking about favorable and unfavorable angle fractures and a number of plates and association between infection and a number of plates. But for this webinar, just for the watchers, that you have two approaches to that parasymphyseal fracture. One is the skeletonization of the nerve, like Dr. Susarla has done here.
That gives you a beautiful view of the inferior border. You have to be very technically meticulous to be able to do that. And it also makes it possible to get direct visualization of your screw fixation posteriorly behind the fracture. If you don't skeletonize the nerve, you can skirt underneath the nerve, but like Dr. Susarla had mentioned earlier, it gives you a very limited view of that posterior plate.
And you have to be very careful that you're not running off the inferior border. And in some cases, you have to go percutaneous to get those posterior screws in because you don't have adequate exposure. Both are very reasonable approaches and both of us do both of them from time to time, depending on the case. But just to let you know, you don't always have to skeletonize the nerve in this case.
Now we've got the fixation. You've closed everything up. What's your postoperative course? Do you continue antibiotics? Do you continue steroids?
Dr. Susarla: I generally don't continue either. Again, I don't know that there's compelling data to suggest that prolonged postoperative antibiotic therapy will meaningfully impact healing in these patients. I think the most important things to emphasize, the patient has to have meticulous oral hygiene in the intraoperative period and really adhere to your prescriptions for reduced jaw activities. So non-chew diet for several weeks and refraining from any activities where they might sustain a recurrent injury to their face for the first few months after healing.
In terms of steroids, again, mixed data. The best data is from postoperative patients undergoing orthognathic surgery which are functionally very similar to this. But the data's somewhat mixed. I don't generally use postoperative steroids for these patients unless there's a significant concern about airway swelling.
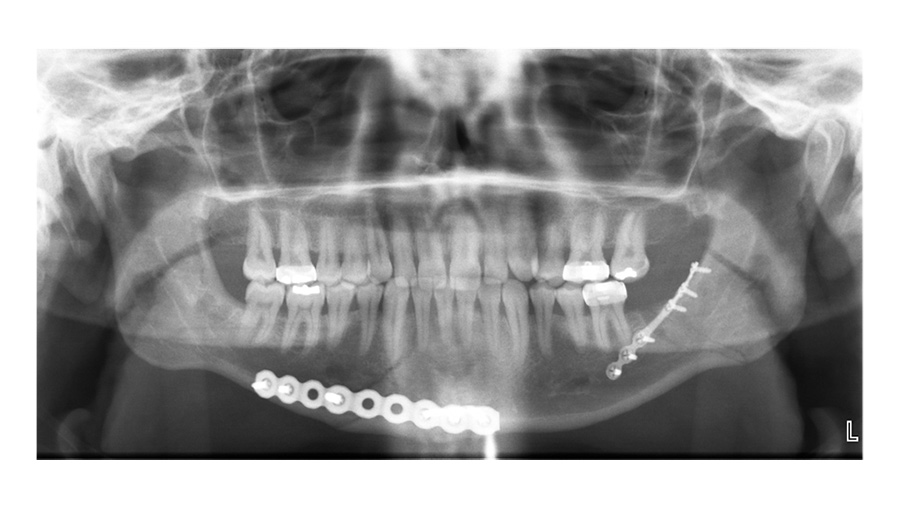
Dr. Hopper: Is this an early postoperative film where you decided to take the Erich arch bars off? Or is this after healing?
Dr. Susarla: This is an early post-operative film, and in this patient, we did take the Erich arch bars off at the end of the case. We were very confident in the stability of the fixation and the patient seemed fairly reliable. So that's a decision I think that every surgeon struggles with at the end of the case like this is, are you confident enough in your fixation to not have the patient in their maxillary fixation postoperatively?
And just as importantly, are you confident enough in the patient's ability to follow your instructions? I think everybody's sort of wrestling with those considerations when deciding to take the arch bars off at the end of the case. There are obviously situations where having the patient in intermaxillary fixation postoperatively is contraindicated.
For example, somebody with an uncontrolled seizure disorder, you would want to make sure that they're not in intermaxillary fixation postoperatively.
Dr. Hopper: That balance between compliance and stability is an experience decision. Last question, do you ever keep a patient in intermaxillary fixation and actually wire them shut for a period of time? Not in the case of kind of condylar fractures, but in patterns such as this. Are there any patient factors that would push you towards maxillomandibular fixation for a period of time?
Dr. Susarla: If I wasn't confident in the quality of the fixation, so if there was significant comminution or the bone quality wasn't great, then I might consider keeping them in intermaxillary fixation for a longer period of time. There's sort of a soft call to keep patients in intermaxillary fixation if you're concerned about their ability to follow your instructions for a non-chew diet.
And I certainly have kept patients in intermaxillary fixation for those periods of time due to that. But I think that's a little bit more difficult to justify in some circumstances. So sometimes it's just a leap of faith that the patient's going to be able to follow your instruction because keeping a patient in intermaxillary fixation, it's certainly easier for us than it is for the patients.
It's something that I talk about with every patient prior to fixation of an occlusal based injury, that there's a chance that they'll wake up with their jaws wired shut. And we talk about what that will entail and what their responsibilities are in the post-operative period and how we follow them. I will say that in patients that I leave in intermaxillary fixation, I tend to see them postoperatively a little more frequently just to make sure that hygiene is okay with the appliances on, that they're able to tolerate a diet -
- most patients lose a little bit of weight - and that they're not having any issues with mucosal inflammation, swelling, lacerations from the wires because those are all things that can make their quality of life bad in the early postoperative period. And most of those are easily addressed as long as you follow the patients closely.
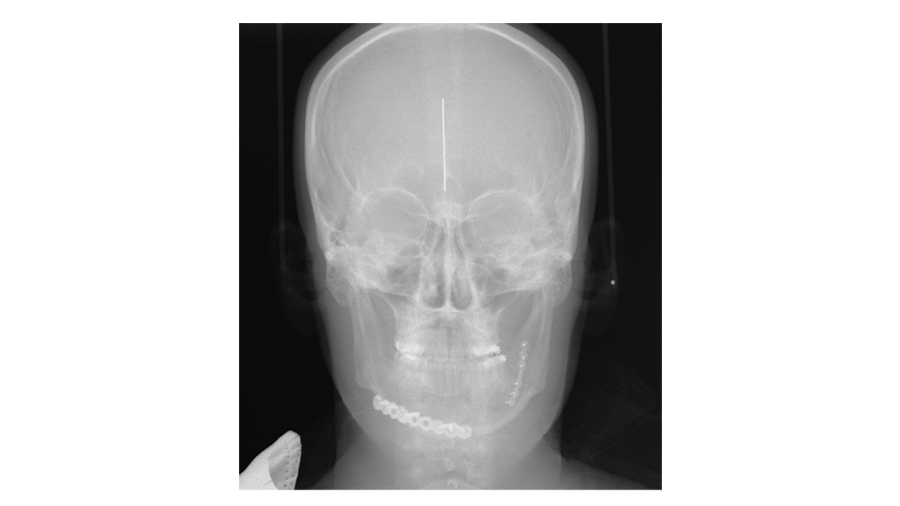
Dr. Hopper: Those are all good points. Obviously, the challenge is you send somebody home in intermaxillary fixation wired shut, you typically have to give them a wire cutter for emergency cases so they can take themselves out of MMF pretty quickly. It's a tough judgment call. And then finally, you decided to use plain films for your postoperative imaging.
So, you have your Panorex - what are you looking for on your PA film here?
Dr. Susarla: The PA film—what I'm looking for is just the splay at the inferior border. One of the advantages of the Panorex is that it's sort of the workhorse for dentoalveolar imaging, particularly for the mandible. It shows you the condyles, it shows you the inferior border, it shows you the teeth, and it can show you the positioning of the fixation relative to the roots of the teeth.
One of the downsides of the Panorex is that it doesn't show you the transverse dimensions. If there's a little bit of lingual splaying, you might not be able to see that as well. My protocol is, particularly in young patients, if there's no compelling reason to get a postoperative CT scan, then I just get plain film imaging to verify to myself that the reduction is adequate and that the hardware looks okay.
And I'd like to get two planes of imaging, so a Panorex, and in this case, a PA ceph[alogram] to be able to show the entirety of what you would imagine three dimensionally or the information you get from a 3D CT scan just with a lower radiation dose.
Dr. Hopper: Well, thank you, Srinu, this has been a lot of fun. To the watchers, this is just a taste of what we'll be discussing in Bellevue. Obviously, in those small group discussions and hands-on workshops and didactic lectures, we'll be touching on complications, management of complications, different approaches, different fracture patterns. We invite you to come and join us in Bellevue, September 11th and 12th.

Computer Aided Maxillofacial Surgery (with Human Anatomical Specimens)
Join world-renowned experts in discussions and lab exercises focused on applying digital tools—such as virtual reconstruction—to complex maxillofacial surgeries
Maxillofacial Reconstruction: A Focus on Ballistic Injury Management (with human anatomical specimens)
Gain practical and immediately applicable skills in managing ballistic maxillofacial injuries from a nationally prominent multidisciplinary faculty (including AO military experts)